Managing Medication for Children and Adolescents with ADHD*
Individuals with attention-deficit/hyperactivity disorder (ADHD) experience chronic problems with inattention and/or hyperactivity-impulsivity to a greater degree than the average person. It is a lifespan disorder, affecting children, adolescents and adults.
Attention-deficit/hyperactivity disorder (ADHD) is a common neurobiological condition affecting 5-8 percent of school age children.1,2,3,4,5,6,7 with symptoms persisting into adulthood in as many as 60 percent of cases (i.e. approximately 4% of adults).8,9 While it has long been thought that boys with ADHD outnumber girls by approximately 3 to 1, recent research shows that the actual numbers may be nearly equal.
Although some media coverage questions the validity of the ADHD diagnosis, medical professional groups such as the American Academy of Pediatrics (AAP), American Academy of Child and Adolescent Psychiatry (AACAP), and American Medical Association (AMA) have recognized the strong scientific evidence for this disorder. “ADHD is one of the best-researched disorders in psychiatry, and the overall data on its validity are far more compelling than for most mental disorders and even many medical conditions,” according to the American Medical Association Council on Scientific Affairs.10
Multiple studies have been conducted to discover the cause of the disorder. The exact causes of ADHD remain elusive, but research indicates that at least three separate yet interactive brain regions have been associated with the condition. Research also clearly indicates that ADHD tends to run in families. More than 20 genetic studies have shown evidence that the disorder is largely an inherited, neurologically-based condition. ADHD is a complex trait, and complex traits are typically the result of multiple interacting genes. Problems in parenting or life situations may make ADHD better or worse, but they do not cause the disorder.
Without early identification and appropriate treatment, ADHD can have serious consequences that include school failure and drop out, depression, conduct disorder, failed relationships, underachievement in the workplace, and substance abuse. When appropriately treated, persons with ADHD can lead productive and satisfying lives.
Diagnosis of ADHD
Determining if a child has ADHD is a multifaceted process. Many biological and psychological problems can contribute to symptoms similar to those exhibited by children with ADHD. For example, anxiety, depression, and certain types of learning disabilities may cause similar symptoms.
There is no single test to diagnose ADHD. Therefore, a comprehensive evaluation is necessary to establish a diagnosis, rule out other causes, and determine the presence or absence of co-existing conditions. Such an evaluation requires time and effort and should include a clinical assessment of the individual’s academic, social and emotional functioning, and developmental level. A careful history should be taken from the parents, teachers and the child, when appropriate. Checklists for rating ADHD symptoms and ruling out other disabilities are often used by clinicians.
There are several types of professionals who can diagnose ADHD, including school psychologists, private psychologists, clinical social workers, nurse practitioners, neurologists, psychiatrists, pediatricians, and other medical doctors. Regardless of who does the evaluation, the use of the Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnostic criteria for ADHD is necessary. An exam by a medical professional is also important and should include a thorough physical examination, including an assessment of hearing and vision, to rule out other medical problems that may be causing symptoms similar to ADHD. In rare cases, persons with ADHD may have a thyroid dysfunction.
Treatment for ADHD
Getting appropriate treatment for ADHD is very important. There may be very serious negative consequences for persons with ADHD who do not receive adequate treatment. These consequences can include low self esteem, social and academic failure, substance abuse, and a possible increase in the risk of antisocial and criminal behavior.
Treating ADHD in children requires medical, educational, behavioral and psychological interventions. This comprehensive approach to treatment is called “multimodal” and consists of parent and child education about diagnosis and treatment, behavior management techniques, medication, and school programming and supports. Treatment should be tailored to the unique needs of each child and family.
Behavior interventions are often a major component for children who have ADHD. Important strategies include being consistent, using positive reinforcement, and teaching problem-solving, communication and self-advocacy skills. Children, especially teenagers, should be actively involved as respected members of the school planning and treatment teams. What We Know #7: Psychosocial Treatment for Children and Adolescents with ADHD, provides more detailed information about psychosocial treatments that have been found helpful for ADHD.
School success may require a range of interventions. Many children with ADHD can be taught in the regular classroom with minor adjustments to the environment. Some children will require additional assistance using special education services. This service may be provided within the regular education classroom or may require a special placement outside of the regular classroom that fits the child’s unique learning needs.
The National Institute of Mental Health conducted a major research study, called the Multimodal Treatment Study of Children with ADHD, involving 579 children with ADHD-combined type. Each child received one of four possible treatments over a 14-month period—medication management, behavioral treatment, combination of the two, or usual community care. The results of this landmark study showed that children who were treated with medication alone, which was carefully managed and individually tailored, and children who received both medication management and behavioral treatment had the best outcomes with respect to improvement of ADHD symptoms.11,12
Combination treatment provided the best results in terms of the proportion of children showing excellent response regarding ADHD and oppositional symptoms and in other areas of functioning (e.g., parenting, academic outcomes).13 Overall, those who received closely monitored medical management had greater improvement in their ADHD symptoms than children who received either intensive behavioral treatment without medication or community care with less carefully monitored medication.
For more information on evaluating treatments, please read What We Know #6: Complementary and Alternative Treatments. This fact sheet provides checklists for spotting unproven remedies and evaluating media reports on treatments.
The Role of Medication
For most children with ADHD, medication is an integral part of treatment. It is not used to control behavior. Medication, which can only be prescribed by certain medical professionals if needed, is used to improve the symptoms of ADHD so that the individual can function more effectively. Research shows that children and adults who take medication for symptoms of ADHD usually attribute their successes to themselves, not to the medication.
Psychostimulant Medications
Psychostimulant compounds are the most widely used medications for the management of ADHD symptoms. Psychostimulant medications were first administered to children with behavior and learning problems in 1937. Despite their name, these medications do not work by increasing stimulation of the person. Rather, they help important networks of nerve cells in the brain to communicate more effectively with each other. Between 70-80 percent of children with ADHD respond positively to these medications. For some, the benefits are extraordinary; for others, medication is quite helpful; and for others, the results are more modest. Attention span, impulsivity, and on-task behavior often improve, especially in structured environments. Some children also demonstrate improvements in frustration tolerance, compliance, and even handwriting. Relationships with parents, peers and teachers may also improve.
Medication does not cure ADHD; when effective, it alleviates ADHD symptoms during the time it is active. Thus it is not like an antibiotic that may cure a bacterial infection, but more like eyeglasses that help to improve vision only during the time the eyeglasses are actually worn. After reviewing the scientific evidence, the AMA reported that “pharmacotherapy, particularly stimulants, has been extensively studied. Medication alone generally provides significant short-term symptomatic and academic improvement” and “the risk-benefit ratio of stimulant treatment in ADHD must be evaluated and monitored on an ongoing basis in each case, but in general is highly favorable.”14
Common psychostimulant medications used in the treatment of ADHD include methylphenidate (Ritalin, Concerta, Metadate, Focalin), mixed salts of a single-entity amphetamine product (Adderall, Adderall XR), and dextroamphetamine (Dexedrine, Dextrostat). Methylphenidate, amphetamine, and mixed salts of amphetamine are now available as both short- and long-acting preparations. Short-acting preparations generally last approximately 4 hours; long-acting preparations are more variable in duration—with some preparations lasting 6-8 hours, and newer preparations lasting 10-12 hours. Of course, there can be wide individual variation that cannot be predicted and will only become evident once the medication is tried. Methamphetamine hydrochloride (brand name Desoxyn) is a central nervous stimulant and is also approved by the FDA for the treatment of ADHD. Because it can be abused or lead to dependence, it is classified as a controlled substance. This medication is not commonly prescribed, except in rare circumstances.
The specific dose and timing of medication must be determined for each individual. However, there are no consistent relationships between height, age and clinical response to a medication. A medication trial is often used to determine the most beneficial dosage. The trial usually begins with a low dose that is gradually increased at 3-7 day intervals until clinical benefits are achieved. It is common for the dosage to be raised several times during the trial.
In addition, the individual is monitored both on and off the medication. For children, observations are collected from parents and teachers, even coaches and tutors, and parent and teacher rating scales are often used. In all cases, the appropriate dose must be tailored to the individual patient and monitored by the prescribing medical professional to make any needed adjustments.
Since effective longer-acting formulations of stimulants have become available in recent years, many children, adolescents and adults have found these preferable. Longer-acting medications may cause fewer “ups and downs” over the day and may eliminate the need for taking additional doses at school or during work. Although there is little research on utilizing short-acting and long-acting medications together, many individuals, especially teenagers and adults, find that they may need to supplement a longer-acting medication taken in the morning with a shorter-acting dose taken in mid to late afternoon. The “booster” dose may provide better coverage for doing homework or other late afternoon or evening activities and may also reduce problems of “rebound” when the earlier dose wears off.
Hundreds of controlled studies involving more than 6,000 children, adolescents and adults have been conducted to determine the effects of psychostimulant medications—far more research evidence than is available for virtually any other medication. There are no studies on the use of psychostimulant medications for more than a few years, but many individuals have been taking these medications for many years without adverse effects. Longer term controlled studies cannot be done because withholding treatment over many years from some patients suffering significant impairments, which is required in a controlled study, would be unethical. Each family must weigh the pros and cons of choosing medication as part of the treatment plan for ADHD.
Nonstimulant Medications
Although stimulants are the best tested and most widely used medications for the treatment of ADHD, some children, adolescents and adults respond just as well or better to treatment with other medications that are not stimulants. Nonstimulants may be used when contraindications to psychostimulant medications exist, psychostimulant medications have been ineffective, unacceptable side effects have resulted, or the individual or child’s parents prefer a nonstimulant for other reasons.
In November 2002, the Food and Drug Administration (FDA) approved a new medication called atomoxetine (Strattera) specifically for ADHD. This medication is neither a stimulant nor an antidepressant. It alleviates inattention and hyperactivity/impulsivity symptoms of ADHD by affecting specific aspects of the norepinephrine system. Atomoxetine has been tested on more than 1,600 children, adolescents and adults. It is a prescription medication, but it is not a controlled substance like a stimulant. This allows medical professionals to give samples and to place refills on the prescriptions. It does not start working as quickly as the stimulants do. Reports suggest that the full effects are often not seen until the person has been taking atomoxetine regularly for 3 or 4 weeks.
Medications initially developed as antidepressants are used less frequently for ADHD but have been shown to be effective. Antidepressants that have active effects on the neurotransmitters norepinephrine and dopamine—i.e. the tricyclics and novel medications like bupropion — can have a positive effect on ADHD symptoms. Antidepressants that only affect the serotonin system—i.e. serotonin selective reuptake inhibitors (SSRIs), such as fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa)—have not been shown to be effective for treating primary symptoms of ADHD but may be effective against co-existing conditions. Clonidine (Catapres) and guanfacine (Tenex) are sometimes prescribed to reduce excessive hyperactivity or severe insomnia in children with ADHD, though these medications have not been shown to be effective for alleviating inattention problems.
Possible side Effects of Medications for ADHD
Most immediate side effects related to these medications are mild and typically short-term. The most common side effects are reduction in appetite and difficulty sleeping. Some children experience “stimulant rebound,” a brief period of negative mood, fatigue, or increased activity when the medication is wearing off. These side effects are usually managed by changing the dose and scheduling for short-acting medications, or by changing to a prolonged-release formulation. Headache and stomachache are occasionally seen; these often disappear with time or, if necessary, a dose reduction. There may be an initial, slight effect on height and weight gain, but studies suggest that ultimate height and weight are rarely affected. For any questions about possible side effects, consult a physician or other medical professional.
Parents sometimes report that medication that had previously worked during childhood no longer works once the child reaches adolescence. Often this problem can be alleviated by dose adjustment or switching to another medication. Adolescence is not usually the time to give up on medical management for ADHD if it was helpful in past years. If such problems occur with your adolescent, discuss your observations and concerns with your medical doctor. A few studies suggest that some children with ADHD reach puberty later than their peers, but this does not appear to be a result of medication treatment.
A relatively uncommon side effect of psychostimulant medications is the unmasking of latent tics—the medical term for involuntary motor movements, such as eye blinking, shrugging and clearing of the throat. Psychostimulant medications can facilitate the emergence of a tic disorder in susceptible individuals. Often, but not always, the tic will disappear when the medication is stopped. For many youth with ADHD, vocal tics (throat clearing, sniffing, or coughing beyond what is normal) or motor tics (blinking, facial grimacing, shrugging, or head-turning) will occur as a time-limited phenomenon. The medications may bring them to notice earlier, or make them more prominent than they would be without medication, but they often eventually go away, even while the individual is still on medication.
Tourette’s syndrome is a chronic tic disorder that involves vocal and motor tics. Experts estimate that 7 percent of children with ADHD have tics or Tourette’s syndrome that is often mild but can have social impact in the severe but rare form, while 60 percent of children with Tourette’s have ADHD. Recent research suggests that the development of Tourette’s syndrome in children with ADHD is not related to psychostimulant medication. However, a cautious approach to treatment is recommended when there is a family history of tics or Tourette’s syndrome, as certain patients will experience worsening of their tics with stimulant treatment. In these cases, treatment with nonstimulant medications may be considered as an alternative.
Starting Medication
Each person considering medication treatment for ADHD should first have a careful, comprehensive assessment to clarify the diagnosis, identify other medical, psychological or learning problems that may be present with ADHD, and learn about ADHD. After the diagnosis has been made, a treatment plan should be developed in consultation with the physician or other medical professional. In this planning session, the patient, family and medical professional can work together to consider the various options for treatment. If medication is going to be used, the medical professional will prescribe a specific medication.
The medication trial should be monitored very carefully, especially in the early weeks of treatment, so needed adjustments can be made to dose and timing. If the first medication tried is not helpful or produces unpleasant side effects, the prescribing professional will probably make adjustments. If the adjustments are not sufficient to bring a good response, another medication option can be tried. Most persons with ADHD respond well to any of the frequently used medications for ADHD. Some respond much better to one than another. If the first medication tried does not produce a satisfactory response, it is usually wise to try a different type of ADHD medication. Ultimately, success with treatment depends on a collaborative effort between the patient and a committed team of caregivers. Medication can help the complete multimodal treatment program be more effective. Medication treatment without monitoring, appropriate education about ADHD, and other appropriate treatment interventions is often not enough to help.
Frequently Asked Questions
Q. How long does it take to achieve a therapeutic dose of medication?
A. The effects of psychostimulant medications are usually noticeable within 30-60 minutes once an appropriate dose for that individual has been found. However, determining the proper dosage and medication schedule for each individual often takes a few weeks. Nonstimulant medications often require several weeks before their full effects can be observed.
Q. As a child grows, will the dosage need to be changed?
A. Not necessarily. Many adolescents and adults continue to respond well to the same doses of psychostimulant medication. However, many others will require higher doses. On the other hand, some children may respond well initially to a low dose of medication and then require a modest dose increase after a few weeks or months once a “honeymoon period” has passed.
Q. Will my child need to take medication forever, even into adulthood?
A. Not necessarily. These medications can be stopped at any time. However, ADHD is a chronic condition. Its severity and developmental course are quite variable in duration and severity. Up to 60 percent of children with ADHD continue to exhibit problematic symptoms into adolescence and adulthood.15,16 For these individuals, continuing effective treatment modalities, including medication, can be helpful.
Q. Should medication only be taken when the child is in school?
A. This should be decided with the prescribing medical professional and the therapeutic team. Children can often benefit from medication outside of school because it can help them succeed in social settings, peer relations, home environment, and with homework. Medication can be of help to children who participate in organized sports and activities that require sustained attention, such as musical programs, debate, or public speaking activities.
Q. What about individuals who do not respond to medication, either psychostimulants or antidepressants?
A. In general, two or three different stimulant medications should be tried before determining that this group of medications is not helpful. Similarly, several different antidepressant medications can also be tried. Most individuals will respond positively to one of these medication regimens. Some individuals, because of the severity of their disability or the presence of other conditions, will not respond. And some individuals will exhibit adverse side effects. In such cases, the entire treatment team—family, medical doctor, mental health professional, and educator—must work together to develop an effective intervention plan. Other medications such as clonidine may be helpful, and occasionally, combinations of medication may be needed. When all medication appears to be ineffective, consideration needs to be given to whether the diagnosis of ADHD is accurate, whether other conditions are affecting functioning, whether appropriate criteria for improvement have been established, and whether objective and accurate feedback is being provided regarding medication efficacy.
Q. Are children who take psychostimulant medications more likely to have substance abuse problems later in life?
A. No. Multiple studies that have followed children with ADHD for 10 years or more support the conclusion that the clinical use of stimulant medications does not increase the risk of later substance abuse.17 In fact, many studies have shown that individuals with ADHD who are not effectively treated with medication during childhood and adolescence have a greatly increased—though not inevitable—risk of developing significant alcohol or drug abuse problems later in life. When treated, the risk of later drug or alcohol problems is reduced to that of non-ADHD individuals.
Although there is potential for abuse when misused, psychostimulant medications do not cause addictions to develop in those being treated appropriately. Unfortunately, research does show that children who demonstrate conduct disorders (delinquent behaviors) by age 10, and who are smoking cigarettes by age 12, are at higher risk for substance abuse in the teenage years, possibly persisting into mid-life. Therefore it is important to recognize this subgroup early and get them involved in an effective multimodal therapeutic program.
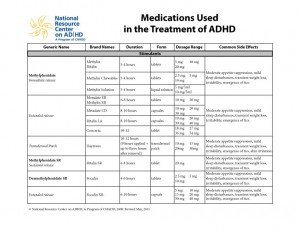
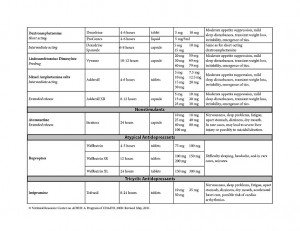
Overview of Medications Often Used in the Treatment of ADHD
This information is provided for educational purposes only. Discuss the specifics of any medication with your physician or medical professional. The names used below are the generic (chemical) names of the compounds, with names of common brands made by different pharmaceutical companies. It should be noted that a number of new medications for the treatment of ADHD are currently being researched and should be available in the near future.
Methylphenidate (Rritalin, MethylinN)
Form: Short-acting tablets administered by mouth. Methylphenidate 5 mg, 10 mg, 20 mg.
Dosage: Very individual. Usually between 2.5–20 mg per dose. Effective dose does not necessarily correlate with age, body weight or severity of ADHD symptoms. Usually the dose starts off small and then is gradually increased to find the most effective dose that will not produce excessive adverse effects.
Duration of Action: Rapid-acting methylphenidate starts to work in 15–20 minutes. Lasts about 3.5–4 hours. Because of its relatively short action, this form of methylphenidate wears off at night and is started again when taken in the morning. Research suggests that short-acting methylphenidate works best for most persons when taken 3 times daily.
Possible Side Effects: Moderate appetite suppression, mild sleep disturbances, transient weight loss, and irritability. “Rebound effect” can occur—anger, frustration or sadness—for a period of about 1 hour when the effect of medication wears off. When the dosage is too high, motor tics may be unmasked, or agitation, depression or lethargy may occur until the dose wears off. These are usually managed by lowering the dose. Tics will usually disappear if the dose is lowered.
Extended Delivery Fofrms of Methylphenidate
To avoid the need for taking short-acting methylphenidate 3–4 times daily, several new long-acting delivery systems have been developed. Each of the systems described below delivers the same medicine used in short-acting methylphenidate tablets, but does so in a way designed to give extended coverage so a child can get through a school day without having to take pills at school.
Concerta, a new osmotic release system for methylphenidate was approved by the FDA in September 2000. This capsule contains three chambers, two filled with different concentrations of methylphenidate and one with a polymer substance that expands when a liquid comes in contact with it. An initial dose of methylphenidate is released from the outer coating soon after the capsule is ingested. As the polymer substance expands in response to liquids absorbed from the digestive tract, it gradually pushes the medication in the two internal chambers out of the capsule, like a piston, through a laser-drilled hole in one end of the capsule. Concerta delivers methylphenidate in an ascending profile. This means that an 18 mg caplet provides 4 mg methylphenidate initially and delivers the rest of the methylphenidate over the course of the day. An 18 mg caplet of Concerta is equivalent to 5 mg of Ritalin given 3 times per day. Concerta is designed to be effective for about 10–12 hours from ingestion, but individual results may vary. Concerta capsules should not be opened or chewed.
Form: 18 mg, 27 mg, 36 mg, 54 mg capsules. (Each 18 mg is equivalent to about 5 mg of short-acting methylphenidate given 3 times over the day.)
Metadate-CD, an extended delivery capsule, was approved by the FDA in April 2001. This capsule contains many tiny beads containing methylphenidate. Beads have various types of coatings so they can release 30% of the methylphenidate dose immediately and then continue to release methylphenidate over an extended period of time designed to cover a school day. Typically, Metadate-CD provides about 8 hours of coverage. These capsules should not be chewed, but the capsules can be opened and sprinkled at the direction of a prescribing medical professional.
Form: 20 mg CD capsule
Ritalin LA, another extended delivery capsule form of methylphenidate. It also consists of two types of tiny beads in a capsule, but is unique in that the amount of methylphenidate released immediately is the same as the amount released 4 hours after the dose. Therefore, Ritalin LA delivers 50% of its methylphenidate initially and 50% approximately 4 hours later. This delivery system mimics Ritalin given twice a day, thus giving approximately 8 hours worth of coverage.
Form: 20 mg, 30 mg, 40 mg capsules.
Methylphenidate SR 20 (methylphenidate sustained release) and Ritalin SR 20, this earliest form of extended release methylphenidate uses a wax matrix to deliver two doses from one pill. An SR 20 tablet releases about 10 mg of methylphenidate within about 1 hour after ingestion and then releases another
10 mg about 3.5 hours later. It is intended to last 6–8 hours. Clinicians report that this preparation works well for some individuals, but is unsatisfactory for many others because it may release too quickly or unevenly. The dosage is prescribed on an individualized basis. Possible side effects are the same as methylphenidate.
Form: 20 mg tablets.
Metadate ER, Methylin ER: similar to the Ritalin SR tablet.
Form: 10 mg, 20 mg tablets.
Mixed Salts of a single-Entity Amphetamine Product
Form: Double-scored tablets administered by mouth.
5 mg, 7.5 mg, 10 mg, 12.5 mg, 15 mg, 20 mg, 30 mg.
Dosage: Very individual.
Duration of Action: Variable. Depending on dose, can last 3.5–8 hours.
Possible Side Effects: Same as methylphenidate.
Adderall XR, extended release capsule was approved by the FDA for ADHD in 2001. Mixed salts of amphetamine used are contained in tiny beads within a capsule. About half of the beads release within an hour; the rest release about 3.5 hours later to provide coverage for approximately 10 hours.
Dosage: Very individual.
Form: Capsules administered by mouth. 5 mg, 10 mg,
15 mg, 20 mg, 25 mg, 30 mg.
Duration of Action: 10-12 hours.
Possible Side Effects: Same as methylphenidate.
Dextroamphetamine (Dexedrine, Dextrostat)
Form: Short-acting tablets administered by mouth. 5 mg, 10 mg tablets.
Dosage: Very individual. Average: 2.5–10 mg.
Duration of Action: Rapid onset of action, 20–30 minutes. Lasts about 4-5 hours.
Possible Side Effects: Same as methylphenidate.
Dextroamphetamine Spansules (Dexedrine), sustained release capsules. Each spansule releases about one-half of its face value dose in about 1 hour and then releases the balance about 3.5 hours later. Thus a 5 mg spansule actually releases 2.5 mg initially and 2.5 mg later. It does not provide the equivalent of 5 mg throughout the duration of its action.
Form: Long-acting, administered by mouth. Dextroamphetamine spansules 5 mg, 10 mg, 15 mg.
Dosage: Very individual. Average: 5–20 mg.
Duration of Action: Very individual. Usually lasts 6–8 hours, but individual reaction may vary from several hours to the whole day.
Possible Side Effects: Same as methylphenidate.
Selective Norepinephrine Reruptake Inhiibitors
Atomoxetine (Strattera) was approved in November 2002 by the FDA for the treatment of ADHD. Atomoxetine acts as a highly specific reuptake inhibitor for norepinephrine and seems to have little effect on other neurotransmitters.
Form: Capsules administered by mouth. 10 mg, 18 mg, 25 mg, 40 mg, 60 mg.
Dosage: Recommended to initiate dose at 0.5 mg/kg/day and titrate to 1.2 mg/kg/day.
Duration of Action: Most patients appear to achieve
24-hour coverage from dosing 1–2 times a day.
Effect: Lower doses may improve ADHD symptoms within several days, but may take 1–3 weeks for full effect. Higher doses may improve depressive symptoms and mood swings.
Possible Side Effects: Nervousness, sleep problems, fatigue, stomach upset, dizziness, and dry mouth. May lead in rare cases to severe liver injury resulting in liver failure if not stopped immediately on finding any liver effects (itching, dark urine, jaundice, right upper quadrant tenderness or unexplained “flu-like” symptoms).
Nortriptyline (various brands), Imiipramane (Tofranil), Desipramine (Norpramin)
Form: Tablets administered by mouth. 10 mg, 25 mg,
50 mg, 100 mg.
Dosage: Very individual.
Duration of Action: Variable. Often has 24-hour effect.
Effect: Lower doses may improve ADHD symptoms within several days, but may take 1–3 weeks for full effect. Higher doses may improve depressive symptoms and mood swings.
Possible Side Effects: Nervousness, sleep problems, fatigue, stomach upset, dizziness, dry mouth, and accelerated heart rate. May affect conduction time of the heart, leading to irregular heart rate. In rare cases, may affect blood count. Should not be abruptly discontinued. Desipramine has been associated with deaths from cardiac problems. Most medical professionals do not use this medication with prepubescent children.
Bupropion (Wellbutrin)
Bupropion is approved by the FDA for the treatment of depression in adults and for nicotine cessation treatment. It is not approved for ADHD.
Form: 75 mg, 100 mg tablets. 100 mg, 150 mg extended release.
Dosage: Very individual.
Duration of Action: About 4-6 hours in short-acting form; 6-8 hours in long-acting form.
Effect: Improves symptoms of ADHD and can affect depressive moods.
Possible Side Effects: Difficulty sleeping and headache.
Antihypertensive Agents
Clonidine (Catapres)
Form: Clonidine is available in patches applied to back of shoulder or tablets administered by mouth. 0.1 mg,
0.2 mg, 0.3 mg.
Dosage: Very individual. The clonidine patch is available in three strengths.
Duration of Action: Patches last 5-6 days. Tablets last 4-6 hours.
Effect: Often will improve excessive hyperactivity or insomnia associated with ADHD, but has not been demonstrated effective for improving inattention symptoms. May decrease facial and vocal tics in Tourette’s syndrome. Often has positive side effect on oppositional defiant behavior and may be beneficial for management of excessive anger.
Possible Side Effects: Major side effect is fatigue, though this will usually disappear over time. Other side effects may include dizziness, dry mouth, increased activity, irritability, or behavior problems. Overdose may cause excessive sedation or other serious problems. Should not be stopped suddenly. A medical professional should be consulted prior to discontinuation of medication to prevent “rebound hypertension” or other effects.
Guanfacine (Tenex)
Form: Tenex is available in 1 mg tablets taken by mouth.
Dosage: Very individual.
Duration of Action: Guanfacine lasts 6-8 hours.
Effect: Often will improve excessive hyperactivity or insomnia associated with ADHD, but has not been demonstrated effective for improving inattention symptoms. May decrease facial and vocal tics in Tourette’s syndrome. Often has positive side effect on oppositional defiant behavior and may be beneficial for management of excessive anger.
Possible Side Effects: Major side effect is fatigue, though this will usually disappear over time. Other side effects may include dizziness, dry mouth, increased activity, irritability, or behavior problems. A medical professional should be consulted prior to discontinuation of medication to prevent “rebound hypertension” or other effects.
Extended Delivery Form of Guanfacine (Iintuniv)
Form: Intuniv is available in 1mg, 2 mg, 3mg, and 4 mg tablets taken by mouth.
Dosage: Very Individual
Duration of Action: 12 ? 24 hours
Effect: Often helps treat symptoms associated with ADHD in children. It is not known if extended delivery guanfacine is effective for adults or children under 6, or if it is safe for children under 6.
Possible side effects: Side effects include low blood pressure, low heart rate, fainting, sleepiness, tiredness, drowsiness, stomach pain, dry mouth, dizziness, decreased appetite, and irritability. Consult with a medical professional if side effects are severe or persistent; do not discontinue medication without consulting a medical professional.
Suggested Reading
American Academy of Child and Adolescent Psychiatry. (2002). Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. Journal of the American Academy of Child and Adolescent Psychiatry, 41(Suppl. 2), 26–49.
Barkley, R. (1998). Attention deficit hyperactivity disorders: A handbook for diagnosis and treatment. New York: Guilford Press.
Brown, T.E. (Ed.). (2000). Attention-deficit disorders and comorbidities in children, adolescents and adults. Washington, DC: American Psychiatric Association Press.
Goldstein, M. (1998). Managing attention deficit hyperactivity disorder in children: A guide for practitioners (2nd ed.). New York: John Wiley & Sons.
Greenhill, L.L., Halperin, J.M., & Abikoff, H. (1999). Stimulant medications. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 503–512.
Pliszka, S.R., Carlson, C.L., & Swanson, J.M. (1999). ADHD with comorbid disorders: Clinical assessment and management. New York: Guilford Press.
Robin, A.L. (1998). ADHD in adolescents: Diagnosis and treatment. New York: Guilford Press.
Spencer, T.J., Biederman, J., Wilens, T.E., Harding, M., O’Donnell, D., & Griffin, S. (1996). Pharmacotherapy of attention-deficit disorder across the life cycle. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 409–432.
Wilens, T.E. (1999). Straight talk about psychiatric medications for kids. New York: Guilford Press.